The intricate dance between hunger and satiety represents one of the most fundamental regulatory processes in human physiology. At the heart of this complex system lie two pivotal hormones: ghrelin, often termed the "hunger hormone," and leptin, the body's primary satiety signal. Their opposing yet complementary actions form a delicate hormonal dialogue that governs energy homeostasis, influencing everything from meal initiation to long-term weight management. The disruption of this precise communication can lead to profound metabolic consequences, making the understanding of their signaling mechanisms not just an academic pursuit but a crucial frontier in addressing modern health challenges like obesity and eating disorders.
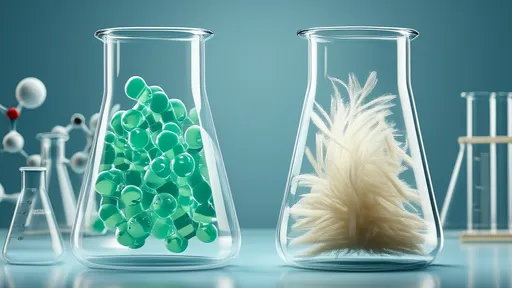
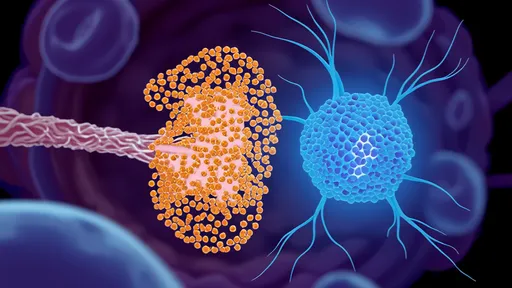
Ghrelin, a peptide hormone predominantly secreted by the X/A-like cells of the gastric fundus, operates as a powerful orexigenic agent—a stimulator of appetite. Its synthesis involves a unique post-translational modification where an octanoic acid side chain is added, a process essential for its biological activity and its ability to cross the highly selective blood-brain barrier. Once released into the bloodstream, ghrelin embarks on a mission to the brain, specifically targeting the arcuate nucleus of the hypothalamus. This region serves as the central processing unit for the body's energy status. Here, ghrelin binds to its receptor, the growth hormone secretagogue receptor (GHS-R1a), setting off a cascade of neural activity that culminates in the intense sensation of hunger. This mechanism is evolutionarily honed to ensure energy intake during periods of caloric deficit, a vital survival tool for our ancestors.
The timing and triggers of ghrelin release are meticulously orchestrated. Circulating ghrelin levels exhibit a clear rhythmic pattern, peaking just before anticipated meal times and dropping precipitously after food consumption. This preprandial rise is a physiological nudge, preparing the body for ingestion. The stomach's emptiness and certain neural signals trigger its secretion, while the presence of food, particularly nutrients like carbohydrates and proteins, swiftly suppresses its production. Beyond its role in short-term hunger signaling, ghrelin exerts broader metabolic influences. It promotes gastric motility and acid secretion, priming the digestive system for the incoming meal. It also interacts with the reward centers in the brain, enhancing the hedonic value of food and making eating a more pleasurable experience, which can sometimes override pure energy needs.
Standing in direct opposition to ghrelin is leptin, the hormone of satiety. Produced primarily by white adipose tissue—body fat—leptin's circulating levels are directly proportional to the body's fat mass. This relationship establishes it as a key indicator of long-term energy reserves. Leptin’s primary mode of action is as a signal of abundance. It travels through the bloodstream to the same hypothalamic centers targeted by ghrelin, binding to specific leptin receptors (Ob-R). Upon activation, these receptors initiate anorexigenic pathways, suppressing appetite and promoting feelings of fullness. It effectively tells the brain, "Energy stores are sufficient; cease seeking food." Furthermore, leptin increases energy expenditure by stimulating thermogenesis and modulating physical activity levels, creating a dual-action approach to maintaining energy balance.
The interaction between ghrelin and leptin is a classic example of a hormonal seesaw. They do not operate in isolation but engage in a continuous push-and-pull dynamic that fine-tunes appetite. Rising ghrelin levels before a meal not only stimulate hunger but also appear to inhibit the action of leptin, temporarily reducing its satiety signal to allow for feeding. Conversely, after a meal, the surge in leptin and other gut-derived satiety hormones works to suppress ghrelin secretion, terminating the hunger signal. This reciprocal relationship ensures a smooth transition between the fasted and fed states. The hypothalamus integrates these opposing signals, along with input from insulin, peptide YY, and other hormones, to generate a coherent response—either to initiate or to cease eating.
However, this elegant system is vulnerable to dysregulation, most notably in the condition of leptin resistance, which is a hallmark of obesity. In a state of excess body fat, leptin levels are chronically high, but the brain becomes desensitized to its signal. The hypothalamic neurons fail to respond appropriately, misinterpreting the body's energy-rich state as one of starvation. This breakdown means the potent satiety signal of leptin is muted, leading to uncontrolled appetite and reduced energy expenditure despite ample—or even excessive—fat stores. Simultaneously, ghrelin dynamics can also be altered. While one might expect ghrelin to be suppressed in obesity, some individuals show blunted post-meal suppression, meaning the "stop eating" signal from leptin is weak, and the "start eating" signal from ghrelin doesn't shut off properly, creating a perfect storm for continued overconsumption.
The implications of understanding the ghrelin-leptin axis extend far beyond basic science, reaching into the realm of therapeutic intervention. The struggle to develop effective, long-term treatments for obesity underscores the complexity of this system. Early hopes for leptin as a simple injectable cure for obesity were dashed when it was discovered that most obese individuals are leptin-resistant, rendering exogenous leptin ineffective. This revelation shifted research focus towards overcoming leptin resistance, perhaps by using combination therapies or enhancing leptin transport across the blood-brain barrier. On the ghrelin front, researchers are investigating ghrelin receptor antagonists—compounds that could block the hunger signal—as potential appetite suppressants. Other strategies aim to mimic the natural post-meal suppression of ghrelin or to modulate the gut microbiome, which is now known to influence the production and signaling of both hormones.
In conclusion, the regulatory dance between ghrelin and leptin is a masterclass in biological balance. Ghrelin acts as the urgent voice of immediate energy need, while leptin provides the calming assurance of long-term energy security. Their signaling mechanisms represent a complex, integrated network designed to preserve energy homeostasis, a system refined over millennia of evolution. The modern prevalence of obesogenic environments, characterized by readily available high-calorie foods and sedentary lifestyles, often overwhelms this ancient regulatory system, leading to dysfunction and disease. Unraveling the precise molecular conversations between these two hormones, and how they are influenced by diet, sleep, stress, and exercise, remains one of the most promising and challenging paths toward developing novel strategies to restore metabolic health and combat the global obesity epidemic.

By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025
By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025
By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025
By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025
By /Aug 29, 2025
By /Aug 29, 2025

By /Aug 29, 2025

By /Aug 29, 2025
By /Aug 29, 2025